Billing is infrastructure: building for value-based care at scale
If you are building a healthcare product in or around value-based care, billing is probably starting to feel harder than you expected.
You might be confident in your clinical model and increasingly focused on outcomes, coordination, and long-term impact. At the same time, questions about reimbursement are becoming more frequent and more specific. How will this care service actually be billed? How do value-based contracts change what needs to be tracked? What happens when payers start asking for more detail?
This is usually when teams realize that billing is not something that can be fully deferred. In value-based care, billing is closely tied to how care, responsibility, and progress toward outcomes are represented across the product, often using leading indicators long before final outcomes are visible. Over time, small assumptions made early about workflows, data, and integrations tend to surface through reimbursement and reporting requirements, especially in specialty care models where rules are more nuanced.
Many healthcare innovators reach this stage while their solution is still taking shape. They are trying to avoid decisions that will quietly limit them later, when billing, reporting, and payer expectations become harder to change.
Billing as the moment of truth in value-based care
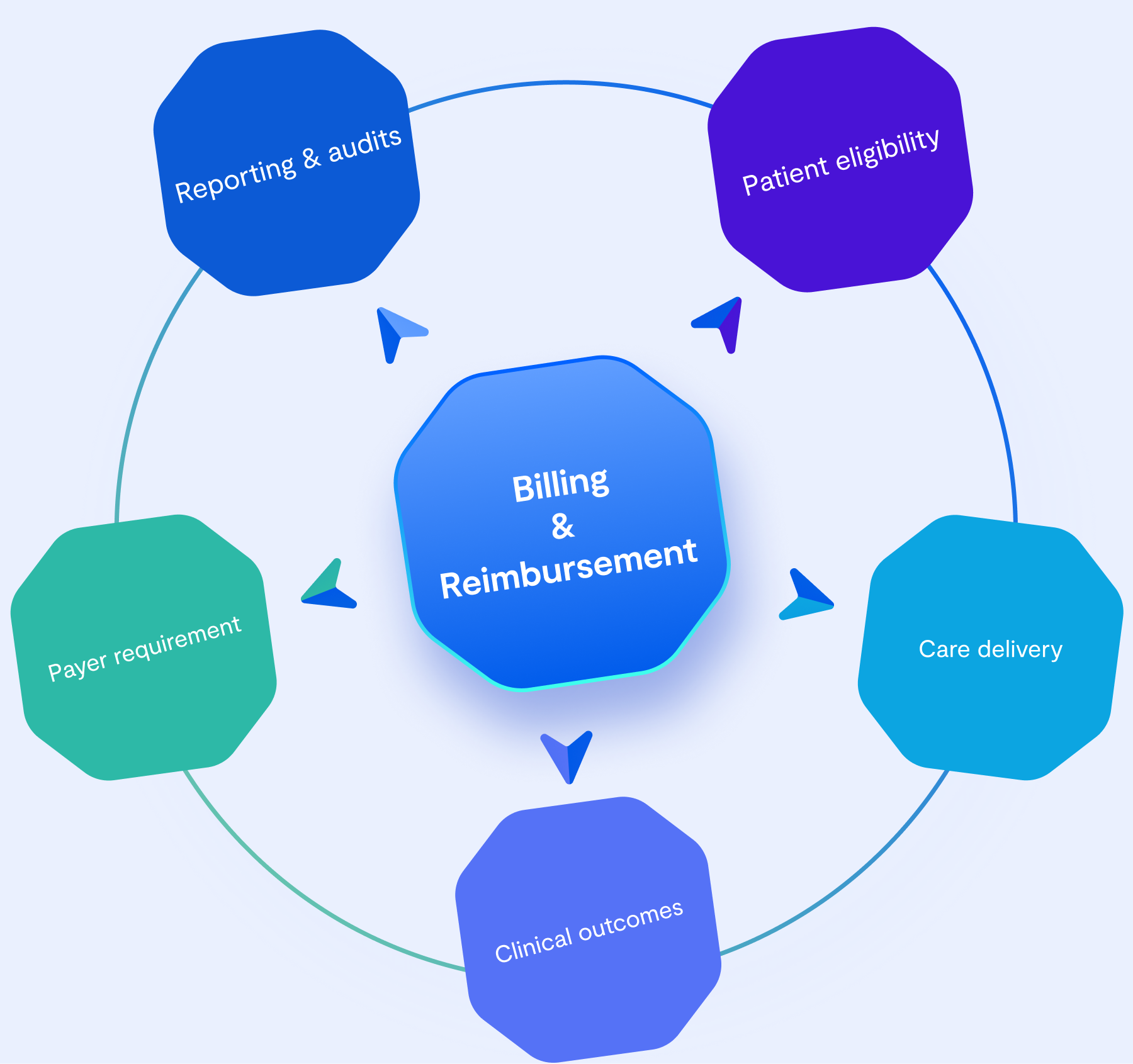
Billing workflows sit at the intersection of clinical data, operational processes, payer requirements, and reporting obligations. In value-based care, this intersection becomes especially sensitive.
In capitated and value-based models, these tensions become harder to ignore. Eligibility rules, attribution logic, and care episode definitions must hold up over longer time horizons, often across multiple systems. What might be manageable ambiguity in fee-for-service contexts becomes more limiting when reimbursement depends on consistent interpretation over time.
Billing surfaces these tensions earlier than most other areas. It forces teams to confront how clearly their system represents care, responsibility, and timing. In that sense, billing often reveals whether the underlying integration approach can support the care model being built.
Fast starts and hidden constraints
Early in a product’s life, speed matters. Off-the-shelf platforms, prebuilt EHRs, clearinghouses, and point integrations allow teams to validate demand and start delivering care quickly. For most innovators, this is the right decision.
These tools reduce upfront complexity and make it possible to focus on patients and providers rather than infrastructure. They also help teams learn what actually matters before committing to deeper investments.
Over time, however, these same choices begin to define what is easy and what is hard to change. Certain workflows become tightly coupled to specific tools. Data models resist adaptation. Billing logic starts to depend on assumptions embedded across multiple systems.
None of this is obvious at the beginning. Constraints tend to appear only once billing, reporting, and value-based requirements become more demanding.
The moment integrations stop scaling with the product
A noticeable shift happens when changes in one area begin to affect others in unexpected ways.
Adjusting a scheduling rule impacts billing eligibility. A reporting requirement exposes gaps in historical data. A payer question triggers a manual investigation across systems. Each system involved may be working correctly on its own, but they often make different assumptions about timing, state, and responsibility.
At this stage, teams spend more time coordinating and reconciling than delivering care. Visibility decreases. Confidence in billing outcomes depends increasingly on manual checks and workarounds. The product still functions, but adapting it becomes slower and riskier.
For leaders, this moment often coincides with deeper engagement in value-based care. It is when billing stops being an operational afterthought and becomes a central concern.

Common risks teams encounter in value-based billing
Value-based care places sustained pressure on billing and data consistency. Outcome attribution requires clarity about when care starts and ends. Eligibility depends on accurate patient and payer data. Reporting demands consistency across long time horizons. When information is fragmented or inconsistently represented, teams struggle to explain results to payers and partners.
In practice, this often leads to manual reconciliation, parallel tracking systems, or ad hoc corrections. These approaches keep operations moving but increase administrative burden and risk as patient volume and contract complexity grow.
These challenges are rarely intentional. They emerge from incremental decisions that were appropriate at the time. Their impact becomes visible only when reimbursement depends on them.
What a healthier path forward looks like
As billing becomes part of the value-based care conversation, some patterns start to separate teams who struggle later from those who retain flexibility.
Teams on a healthier path tend to make a few practical moves early on. These are not about final solutions, but about reducing ambiguity before it becomes expensive.
Common patterns include:
Making care definitions explicit early: Teams align internally on what constitutes a care episode, what outcomes matter, and where responsibility begins and ends, before encoding those ideas into billing workflows.
Treating clinical and billing coding as part of the product: In value-based care, coding influences how care is measured, reported, and evaluated. Healthier teams recognize that coding decisions affect analytics, performance tracking, and payer conversations, not just claims submission.
Separating learning from automation across billing and reporting: Instead of fully automating billing and reporting logic too early, teams focus on visibility first. They make it possible to inspect how data flows from care delivery to coding, billing, and reports, leaving room to adjust as contracts and requirements evolve.
Designing reporting with payer scrutiny in mind: Teams expect that value-based models will require more detailed, longitudinal reporting. They plan for this by ensuring that the data needed to explain outcomes, utilization, and performance can be accessed and interpreted consistently over time.
Avoiding one-off billing decisions: They resist shortcuts that solve a single reimbursement case but create long-term rigidity, especially in specialty and value-based contexts.
Expecting change as a given: Contracts evolve, reporting requirements shift, and care models mature. Teams plan for this reality instead of assuming stability.
These behaviors don’t eliminate complexity, but they help teams preserve room to adapt as billing requirements grow more demanding.
Finding the right direction before billing locks you in
For teams building toward value-based care, the goal is not to get billing “right” from the start. The goal is to make early decisions that remain workable as care models, coding practices, payer expectations, and reimbursement structures evolve.
Billing workflows tend to solidify how care is grouped, how services are coded, and how outcomes are reported. Over time, these elements become intertwined. When they are aligned early, teams gain confidence and flexibility. When they are not, adjustments later tend to require manual work, parallel systems, or re-interpretation of historical data.
Teams that navigate this transition more confidently tend to focus on a few foundational principles:
- Decide which assumptions you are willing to revisit later.
Some early decisions around care definitions, coding practices, and reporting structures are easier to change than others. Being explicit about which ones are provisional helps teams avoid accidental lock-in.
- Design for traceability, not just reimbursement
Healthier approaches make it easier to explain how a reported outcome, metric, or payment was derived, months after care was delivered.
- Expect reporting requirements to evolve
Value-based care introduces new measures, performance frameworks, and payer questions over time. Early integration decisions should support iteration rather than assuming reporting needs will stay static.
Seen this way, choosing a direction for billing is less about selecting tools and more about establishing a foundation where care, coding, billing, and reporting can evolve together without constant rework.
Building billing foundations with the right support
As billing becomes more central to value-based care, teams often find themselves balancing care delivery, reimbursement requirements, and operational clarity at the same time.
The teams that move forward with confidence are rarely the ones who attempt to solve everything upfront. Instead, they seek clarity early, validate assumptions, and put guardrails in place that allow them to adapt without disrupting care delivery.
This is where working with experienced healthtech partners can make a meaningful difference. At Vinta, we work with teams who are building toward value-based care and want to approach integrations thoughtfully. We help clarify risks, structure early integration decisions, and design foundations that support healthcare solutions along the way.

.webp)










%201.webp)
