The hidden gaps of off-the-shelf EHRs in specialty care
If you’ve searched for an off-the-shelf EHR because your project demanded an easy win, you probably remember the pitch: fast setup, low upfront cost, and open APIs that connect to almost everything, right?
Sometimes, the promise holds up; other times, clients realize they need very specific workflows. Specialty care programs are built around interdisciplinary collaboration, compliance-heavy processes, and nuanced patient journeys. Those don’t fit neatly into general-purpose templates or rigid data models.
An extra click here, a missing field there… what starts as a minor friction can slowly turn into operational debt. Clinicians begin to improvise by using a mix of tools, teams lose alignment, and data quality declines just when you need it most.
To put it in a few words: off-the-shelf EHRs are built for broad coverage. Specialty care, on the other hand, often requires a deeper level of adaptability. In this article, we’ll uncover the hidden gaps behind ready-made systems, show how to recognize when your EHR no longer fits, and explore practical paths to modernization or custom development.
Let’s get to it.
The most common EHR limitations
Even the most polished off-the-shelf platforms eventually hit a ceiling when they’re used for specialty care. The challenge isn’t in how these systems are built, but in what they’re built to serve. Their strength lies in wide applicability and usage readiness, but that same universality can make it harder to reflect the nuanced workflows of specialty care.
Below are the most common limitations that tend to surface once a care model becomes more sophisticated or interdisciplinary.
Customization that stops where your workflow begins
Most generalist EHRs let you rename fields or rearrange templates, but real customization ends at the surface. Specialty workflows often rely on conditional logic, multi-step approvals, or multi-role documentation chains that can’t be modeled without developer access. The result: providers force their care model into the system’s logic instead of the other way around.
Collaboration that lives outside the EHR
Integrated care teams demand continuous communication between clinicians, care Ops, and administrative staff. Collaboration features are often limited: few tools offer shared task management or contextual messaging inside the EHR, which makes coordinated care harder to track.. When collaboration moves to spreadsheets or chat apps, compliance and context go with it.
Integrations that exist on paper, not in practice
APIs are often advertised as “open,” yet they’re incomplete, poorly documented, or gated behind enterprise contracts. Integrating labs, payers, or scheduling systems becomes a series of manual workarounds. Product teams waste time reconciling inconsistent data instead of improving the clinical experience.
Reporting that tells you little about care quality
Ready-made analytics modules surface visit counts and billing data, but not the metrics specialty programs truly care about—progress tracking, adherence, outcome scores. Without the ability to model your own datasets, insights stay shallow and disconnected from clinical impact.
Hidden costs and slow vendor response
Initial licensing may look affordable, but once you need additional users, storage, or integrations, costs escalate quickly. Add slow support queues and long change-request cycles, and even basic updates feel like enterprise-level projects.
Red flags that your EHR no longer fits
Recognizing when to move on from an EHR is not that obvious. Most teams don’t wake up one day and decide to migrate. In fact, they slowly adapt around limitations until the workarounds become unsustainable.
If any of the following feel familiar, it’s a sign your system is holding your organization back.
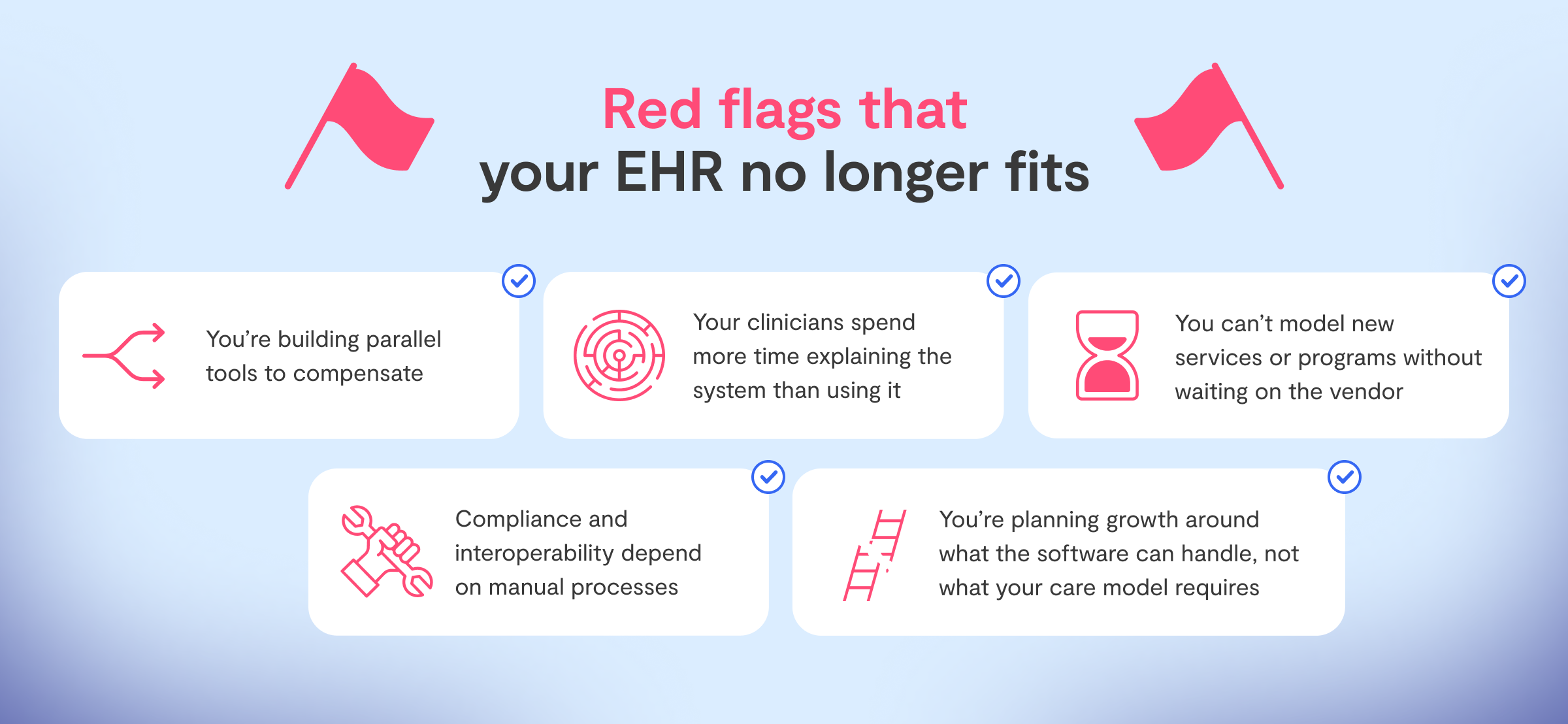
- 🚩 You’re building parallel tools to compensate
Your operations team manages dashboards in Retool, and clinicians keep notes in Google Sheets because the EHR can’t capture what matters. Every workaround fragments your data and adds compliance risk.
- 🚩 Your clinicians spend more time explaining the system than using it
When onboarding new staff requires a “how-to” on getting around bugs or hidden screens, usability debt has replaced clinical efficiency.
- 🚩 You can’t model new services or programs without waiting on the vendor
Whether it’s group therapy sessions, remote monitoring, or custom intake forms, every iteration stalls behind ticket queues and rigid templates, making innovation dependent on vendor roadmaps.
- 🚩 Compliance and interoperability depend on manual processes
Sensitive information travels across email attachments or untracked exports because your EHR doesn’t integrate securely with labs, payers, or other systems.
- 🚩 You’re planning growth around what the software can handle, not what your care model requires
When product decisions are constrained by EHR limitations instead of clinical priorities, it’s a clear sign the system has outlived its purpose.
What happens when you outgrow your off-the-shelf EHR
For Rewind, a platform designed to help individuals achieve remission from Type 2 diabetes, speed mattered most in the early days. Their team needed to document sessions, track progress, and start serving patients quickly. A ready-made EHR seemed perfect for that moment: fast setup, low cost, and “enough” flexibility to get things moving.

But as the care model evolved, so did the friction. Clinicians wanted better ways to record progress and outcomes. Care coordinators needed to collaborate on patient journeys that crossed multiple touchpoints. None of this fit the structure of their existing EHR, and vendor customization moved too slowly to keep up. The system that once made things faster has now added delays to every new idea.
That is when Rewind partnered with Vinta to step back and rethink the foundation. Together, we ran a Healthcare Discovery to map every workflow, integration, and reporting requirement before making any technical decisions. The outcome was a modular platform built on FHIR and Medplum, designed from the ground up to support collaboration, interoperability, and ongoing growth.
The lesson is simple but crucial for any specialty-care organization: migration is not about replacing one tool with another. It is about aligning your technology with the way you care for people.
What specialty care really needs from an EHR
As care models grow beyond standard templates, many off-the-shelf EHRs start showing the limits of their design focus. They excel at billing and record-keeping, but may need complementary layers to fully support coordinated, specialty-driven care. Specialty programs need something more purposeful — software that adapts to how people work together, not software that forces everyone to work around it.
Here is what that looks like in practice:
Interoperable, API-first, and FHIR-native architecture
Data must flow freely across systems. When labs, pharmacies, payers, or external partners connect through reliable APIs, teams can automate key steps and reduce errors that come from manual handoffs. FHIR-native foundations ensure that information is not just exchanged but actually understood across platforms.
Flexible customization that mirrors real workflows
Every specialty operates differently. The right EHR should let teams shape data models, forms, and permissions around their specific processes, from intake to follow-up. It should feel like an evolving product, one that grows with your care model instead of constraining it.
Collaboration built into the experience
Care delivery is rarely a solo act. Multi-disciplinary teams need shared notes, task assignment, and contextual messaging inside the system itself. When collaboration happens within the EHR, not outside it, care plans stay cohesive and compliant.
Reliable reporting and registries
Specialty care depends on outcomes. Metrics should be traceable to clinical actions, not buried in exports or BI dashboards that live in another tool. An effective EHR enables teams to measure adherence, impact, and operational performance directly within their workflows.
A unified, sustainable environment
When every function, like scheduling, messaging, documentation, and analytics, runs through disconnected apps, context disappears. The right foundation consolidates these touchpoints in one environment, minimizing operational friction and long-term maintenance costs.
Specialty care does not need more software. It needs systems that truly reflect the care model itself.
Moving beyond limitations
When an EHR starts to slow your business down, the right question shouldn't be “What's wrong?” but rather “What now?”. Replacing an entire system is costly and disruptive, yet staying put often means layering new tools on top of old problems.
The truth is that not every EHR failure calls for a full rebuild. What matters is identifying whether your challenges come from configuration, architecture, or strategy. That is why we approach every engagement with structured evaluation before any line of code is written.
Healthcare Discovery
This is where clarity begins. Through structured workshops and hands-on analysis, we help teams understand where their current EHR supports the care model — and where it quietly undermines it. The outcome is a roadmap that separates short-term fixes from long-term needs, reducing the risk of another costly cycle of patchwork solutions.
EHR Modernization
When the foundation is viable, modernization allows you to build on it with purpose. We enhance interoperability, automate administrative flows, and extend reporting capabilities so the platform supports multidisciplinary collaboration without losing stability. It is how organizations move from “working around” their system to actually building on it. Learn more here →
Custom EHR Development
When limitations are structural, a clean slate is often the most sustainable choice. Our teams design and build FHIR-native, API-first systems tailored to your workflows, compliance requirements, and long-term scalability. This approach creates not just an EHR, but a flexible foundation that can evolve with your organization’s mission. Learn more →
Whether modernization or custom development is the right path, the goal is the same: transforming your EHR from a daily constraint into a long-term enabler of better care.
Time to turn limitations into opportunities
Off-the-shelf systems are excellent for getting started, but specialty care rarely stands still. As your workflows evolve, your technology should evolve too, so recognizing these gaps early prevents bigger problems later on.
At Vinta, we see every limitation as a signal. It points to something worth improving. If your EHR feels like it no longer fits, the next step is simple: gain clarity before making another big investment.
Our Healthcare Discovery process helps specialty care organizations understand where their system stands today, what modernization would truly solve, and what opportunities might be waiting behind the current friction.











%201.webp)
